Who we help
Nurse professional development and residency
- Enrich curricula and competencies by offering step-by-step prompts that guide the user through the EBP process.
- Decrease workload with one simple solution that serves as the repository for the residency program’s projects.
- Gain high-level oversight and real-time tracking of resident projects to decrease duplication of effort.
- Empower and retain proficient practicing nurses who climb the clinical ladder.
Nurse leadership, Hospital QI, and Magnet® staff
- Advance training and skills by offering built-in guidance for staff at all levels by aggregating and synthesizing the latest evidence to ensure quality projects.
- Strengthen collaboration and eradicate work silos to encourage a culture of EBP and QI.
- Save time and resources by giving managers high-level, real-time oversight of the QI, EBP, and status checking of projects.
- Decrease the amount of manual effort for Magnet®️ application by organizing and storing data for survey reports.
Nurse leadership, Hospital QI, and Magnet® staff
- Advance training and skills by offering built-in guidance for staff at all levels by aggregating and synthesizing the latest evidence to ensure quality projects.
- Strengthen collaboration and eradicate work silos to encourage a culture of EBP and QI.
- Save time and resources by giving managers high-level, real-time oversight of the QI, EBP, and status checking of projects.
- Decrease the amount of manual effort for Magnet®️ application by organizing and storing data for survey reports.
Featured cases and articles for Ovid Synthesis
How an improvement solution can empower staff to deliver the best patient care
Organization-wide,
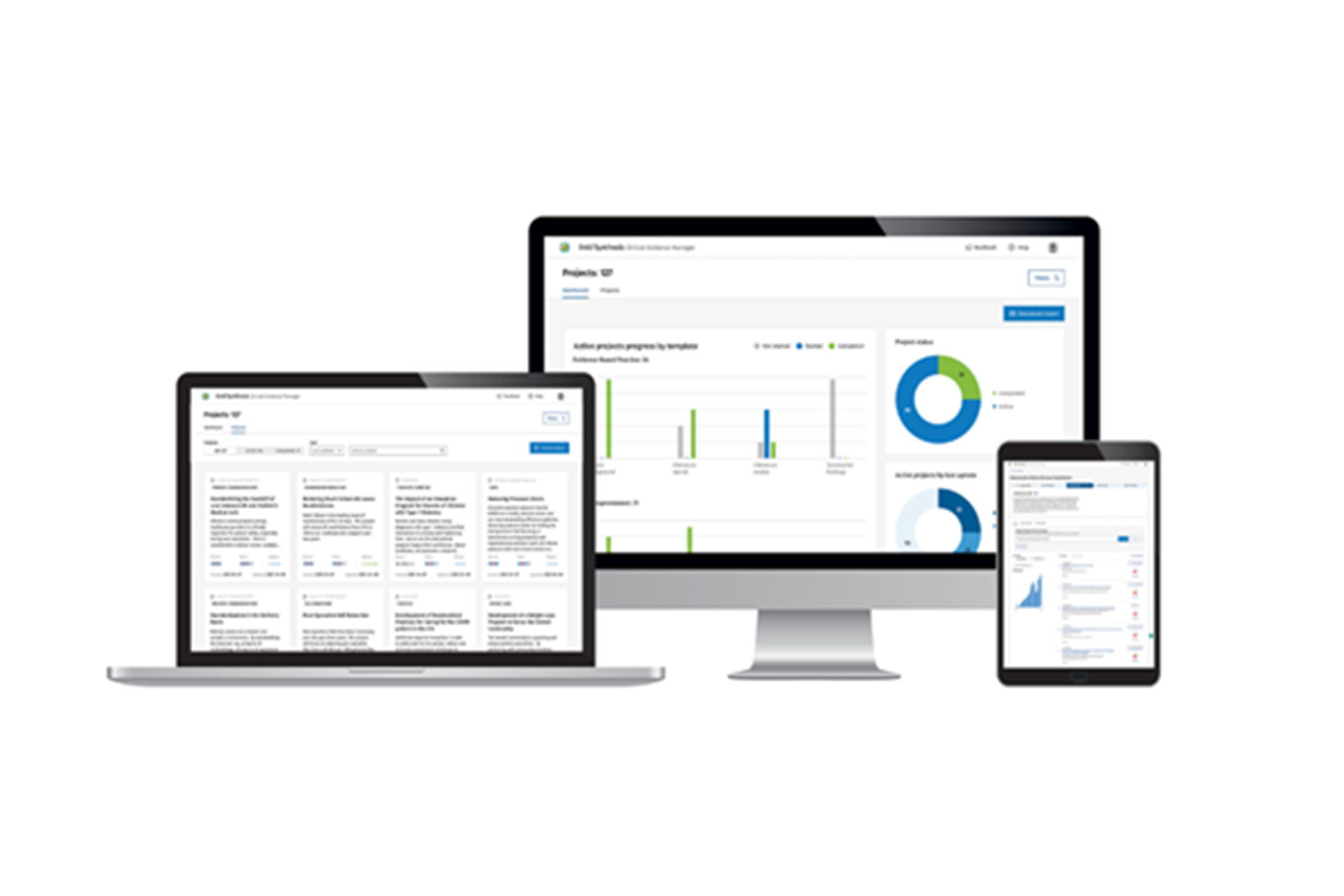
Ovid Synthesis
puts the power of
EBP into clinicians’
hands while ensuring
standard workflow
is followed which
ensures evidencebased outcomes.
Download WhitepaperMeasure ROI with Ovid Synthesis
The Ovid® Synthesis ROI functionality automatically aggregates ROI data across projects to align with institutional goals and provide justification for program and departmental investment.
Download Fact SheetHow one hospital is accelerating EBP and QI: A Portland VA Case Study
Amid Magnet® redesignation, the Portland VA looks to Ovid Synthesis to solve cross-system challenges.
How a University and health system bridge the academia-practice gap with Ovid Synthesis
Learn how University of Alabama implemented Ovid Synthesis to facilitate their QI to support both learners and faculty.
Preparing tomorrow’s nurses – a strong technology backbone streamlines research to support EBP and QI
Explore how to ensure academic excellence within your program by leveraging evidence-based practice technological infrastructure.
Prepare nurse residents for evidence-based practice with technology tools
Discover new tools to equip your nurse residents with proficient research knowledge and skills for practice.
How a large healthcare system enriched the quality of education in its residency program
Learn how Ovid Synthesis solved EBP and QI challenges for AdventHealth.
Explore how to implement evidence-based care to elevate clinical and financial outcomes
Learn how investing in an innovative EBP and QI solution can lead to significant return on investment along a healthcare organization’s journey to achieving nursing excellence.
Showcase the value of the library with an innovative research solution
Discover how the library can prove its value beyond search with new technology that increases visibility at an institutional level.
Request a Demo
Contact us to learn how we can help you improve the standards of quality healthcare.
Ovid Synthesis bridges the EBP theory-to-practice gap, streamlines the process from PICOT question to project completion, and empowers users to lead, using the most current evidence.
We aim to embed EBP into every aspect of our work, thanks to Ovid Synthesis.
Technology like Ovid Synthesis can transform the teaching and learning experience.